Health Committee Recap:
The CSG West Health Committee, chaired by Senator Rochelle Nguyen (NV) and Representative Steven Eliason (UT), led a robust conversation on the increased recognition of anxiety, depression, addiction, and PTSD has resulted in a closer examination of the use of psychedelics, psilocybin therapy, and collaborative care.
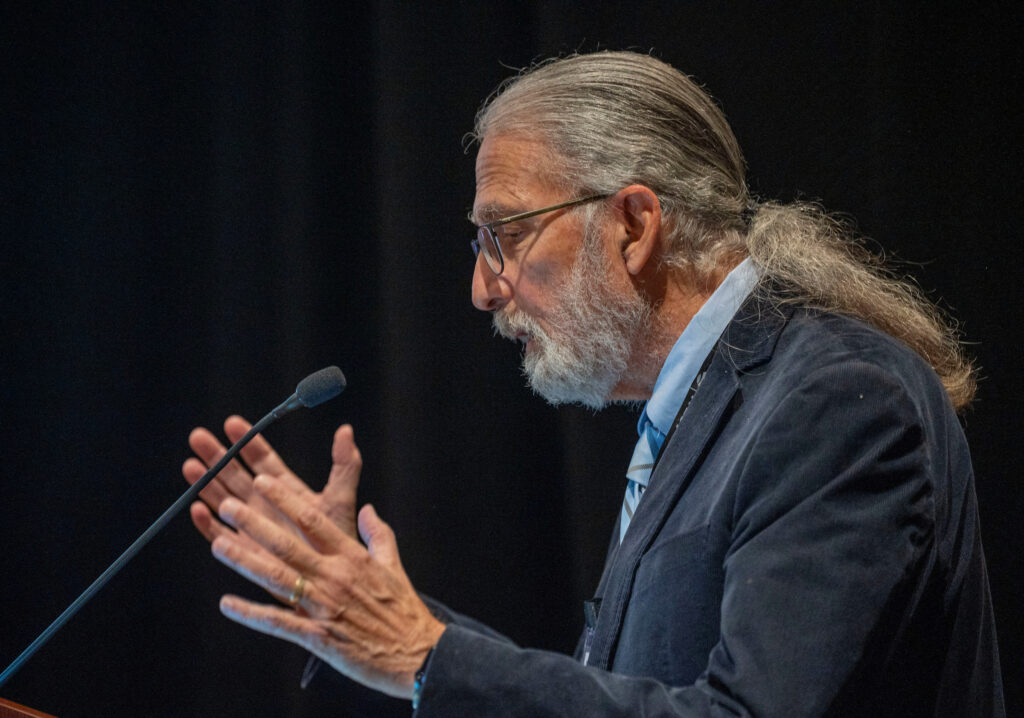
Safety Considerations in Psychedelic Clinical Trials
Charles S. Grob, MD, Harbor-UCLA, gave an overview of safety considerations in psychedelic clinical trials. He emphasized that the research is in its infancy, not everyone is a good candidate for this type of treatment, and guardrails must be implemented as legislation proceeds. Precipitating factors to consider include:
- Severe underlying vulnerability
- Biological family history of severe mental illness
- Excessive hallucinogen use
- Poor support systems/environmental instability
- History of untreated, chronic PTSD.
Psychedelics Healing Veterans
Jon Dalton, President and Legislative Policy Advisor, Nevada Coalition for Psychedelic Medicines (CW04 Retired), shared his story of PTSD and led an open conversation on psychedelics and how to move forward to continue to treat veterans.
Washington State’s Legislative Progress on Psilocybin Research and Supported Use
Senator Jesse Salomon (WA) led a discussion on legislative efforts to find a path forward on safe and bi-partisan efforts to allow for the use of psychedelics and psilocybin to address addiction and mental health issues.
Collaborative Care
Representative Steven Eliason continued the conversation on mental health. The emphasis was on the increase in substance abuse and suicide and the decrease/shortage of mental health care providers. Salient data points included:
- 60% of patients who meet the criteria for a psychiatric disorder in primary care clinics do not get any treatment within one year.
- Only 20% of patients who receive psychotropic medication in primary care settings improve.
- 45% of individuals who died by suicide saw their primary care provider in the past month